After Halloween, I came across this spooky article in Science describing yet anoth
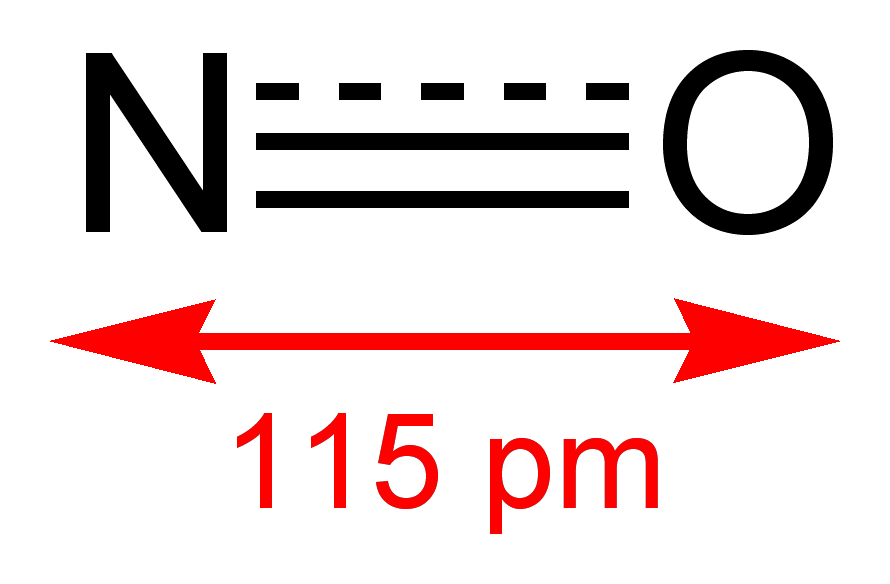 er way bacteria are dodging antibiotics. Don’t worry, there’s a silver lining! Gusarov and his colleagues may have found a new target for the antibiotic industry, bacterial nitric oxide synthase (bNOS).
er way bacteria are dodging antibiotics. Don’t worry, there’s a silver lining! Gusarov and his colleagues may have found a new target for the antibiotic industry, bacterial nitric oxide synthase (bNOS).It turns out bNOS is present in numerous Gram-positive species, along with some Actinobacteria and even a member of the Archaea (Natronomonas pharaonis, a resident of pH 11 soda lakes in Kenya and Egypt that likes its NaCl to the tune of 3.5 M). While most of the organisms cited in the paper are nonpathogenic, there are a few notable nasties you might recognize, including Bacillus anthracis (anthrax) and Staphylococcus aureus (MRSA). Though less extravagantly equipped than its eukaryotic cousins, bNOS is still able to produce NO/NO+ with the help of cellular reductases. The common reason for bNOS in all these species remains elusive, but Gusarov may be onto something with his antibiotic-killer theory.
Using three different but similar antimicrobials (acriflavine [ACR], pyocyanin [PYO] and cefuroxime [CEF]), Gusarov demonstrates that bNOS provides two important survival mechanisms: 1) direct detoxification of some antimicrobials the and 2) destruction of reactive oxygen species. He performed a screen of B. subtilis growth rates against 21 different antimicrobials and chose 3. The first two are both highly hydrophobic and contain conjugated 6-membered rings, making them likely DNA intercalators. However, while ACR is a man-made drug that fights sleeping sickness, PYO is a natural bacteriocin produced by Pseudomonas aeruginosa and seems to be a natural weapon against competitors in the soil. The third, a cephalosporin, is a modified version of the well-known beta-lactam group of antibiotics and was developed in the 1970’s in response to growing concern over beta-lactamases.
Gusarov moves on to show that ACR—but neither PYO nor CEF—is directly neutralized by NO/NO+, specifically at its dangerous arylamino groups. The other, and far more important, function o
.jpg) f bNOS is revealed when Gusarov starts monitoring the levels of superoxide dismutase (SodA) transcription in a B. subtilis nos null mutant. Bacteria without bNOS fail to boost transcription of sodA in late log phase, rendering them helpless against the onslaught of radicals and oxidizers present in stationary phase. As a result, mutant B. subtilis reaches stationary phase at ~60% of the cell density reached by WT.
f bNOS is revealed when Gusarov starts monitoring the levels of superoxide dismutase (SodA) transcription in a B. subtilis nos null mutant. Bacteria without bNOS fail to boost transcription of sodA in late log phase, rendering them helpless against the onslaught of radicals and oxidizers present in stationary phase. As a result, mutant B. subtilis reaches stationary phase at ~60% of the cell density reached by WT.Taken together, these data cast bNOS as a major factor in the cellular response to reactive oxygen species, with a minor talent for direct NO/NO+ neutralization of antimicrobials. Perhaps the original role of bNOS was to help prepare the cell for the stressful conditions of stationary phase and keep up with competitors, but now it seems that the protein can double as a shield against a plethora of antimicrobials. If we are able to find a bNOS inhibitor in the future, it might help decrease bacterial load in non-Gram-negative infections by supplementing conventional treatments, in the style of augmentin. Furthermore, given the high involvement of ROS in the body’s innate immune response, taking out bNOS could make our natural defenses all the more potent.
Source
Gusarov I, Shatalin K, Starodubtseva M, & Nudler E (2009). Endogenous nitric oxide protects bacteria against a wide spectrum of antibiotics. Science (New York, N.Y.), 325 (5946), 1380-4 PMID: 19745150
Other Articles of Interest
Out With the Bad: Efflux in Klebsiella pneumoniae
Antibiotic Treatment: Increasing the Rates of Genetic Exchange
Utilizing Natural Killers: Phage Based Antimicrobials



No comments:
Post a Comment